Content
If breathing is disturbed, the patient is artificially ventilated or mechanically ventilated. It is used for life support when the patient cannot breathe on his own or when he lies on the operating table under anesthesia that causes a lack of oxygen. There are several types of mechanical ventilation - from simple manual to hardware. Almost anyone can handle the first one, the second one requires an understanding of the device and the rules for using medical equipment.
What is artificial lung ventilation
In medicine, mechanical ventilation is understood as the artificial blowing of air into the lungs in order to ensure gas exchange between the environment and the alveoli. Artificial ventilation can be used as a resuscitation measure when a person has serious violations of spontaneous breathing, or as a means to protect against lack of oxygen. The latter condition occurs during anesthesia or diseases of a spontaneous nature.
Forms of artificial ventilation are hardware and direct. The first uses a gas mixture for breathing, which is pumped into the lungs by a machine through an endotracheal tube. Direct implies rhythmic contraction and unclenching of the lungs to ensure passive inhalation-exhalation without the use of a device. If an "electric lung" is applied, the muscles are stimulated by the impulse.
Indications for IVL
To carry out artificial ventilation and maintain the normal functioning of the lungs, there are indications:
- sudden cessation of blood circulation;
- mechanical asphyxia of breath;
- injuries of the chest, brain;
- acute poisoning;
- a sharp decrease in blood pressure;
- cardiogenic shock;
- asthma attack.
After operation
The endotracheal tube of the ventilator is inserted into the patient's lungs in the operating room or after delivery from it to the intensive care unit or the ward for monitoring the patient's condition after anesthesia. The goals and objectives of the need for mechanical ventilation after surgery are:
- exclusion of expectoration of sputum and secretions from the lungs, which reduces the frequency of infectious complications;
- reducing the need for support of the cardiovascular system, reducing the risk of lower deep venous thrombosis;
- creating conditions for feeding through a tube to reduce the frequency of gastrointestinal upset and return normal peristalsis;
- reduction of the negative effect on skeletal muscles after prolonged action of anesthetics;
- rapid normalization of mental functions, normalization of the state of sleep and wakefulness.
With pneumonia
If the patient develops severe pneumonia, this quickly leads to the development of acute respiratory failure. Indications for the use of artificial ventilation in this disease are:
- disorders of consciousness and psyche;
- lowering blood pressure to a critical level;
- intermittent breathing more than 40 times per minute.
Artificial ventilation is carried out in the early stages of the development of the disease in order to increase work efficiency and reduce the risk of death. IVL lasts 10-14 days, 3-4 hours after insertion of the tube, a tracheostomy is performed. If the pneumonia is massive, it is carried out with positive end-expiratory pressure (PEEP) for better lung distribution and reduced venous shunting. Together with the intervention of mechanical ventilation, intensive antibiotic therapy is carried out.
With a stroke
The connection of mechanical ventilation in the treatment of stroke is considered a rehabilitation measure for the patient and is prescribed for indications:
- internal bleeding;
- lung damage;
- pathology in the field of respiratory function;
- coma.
During an ischemic or hemorrhagic attack, shortness of breath is observed, which is restored by a ventilator in order to normalize the lost brain functions and provide the cells with a sufficient amount of oxygen. They put artificial lungs for a stroke for up to two weeks. During this time, a change in the acute period of the disease passes, swelling of the brain decreases. Get rid of the ventilator if possible, as soon as possible.

Types of IVL
Modern methods of artificial ventilation are divided into two conditional groups. Simple ones are used in emergency cases, and hardware ones - in a hospital setting. The former can be used if a person does not have independent breathing, he has an acute development of respiratory rhythm disturbance or a pathological regimen. Simple methods include:
- mouth to mouth or mouth to nose- the head of the victim is thrown back to the maximum level, the entrance to the larynx is opened, the root of the tongue is displaced. The person conducting the procedure stands on the side, compresses the wings of the patient's nose with his hand, tilting his head back, and holds his mouth with his other hand. Taking a deep breath, the rescuer presses his lips tightly to the mouth or nose of the patient and exhales sharply with energy. The patient must exhale due to the elasticity of the lungs and sternum. Simultaneously conduct a heart massage.
- Using S-duct or Reuben bag. Before use, the patient needs to clear the airways, and then press the mask tightly.
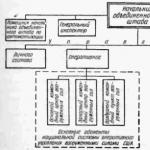
Ventilation modes in intensive care
The artificial respiration apparatus is used in intensive care and refers to the mechanical method of ventilation. It consists of a respirator and an endotracheal tube or tracheostomy cannula. For an adult and a child, different devices are used, differing in the size of the device being inserted and in the adjustable respiratory rate. Hardware ventilation is carried out in a high-frequency mode (more than 60 cycles per minute) in order to reduce the respiratory volume, reduce pressure in the lungs, adapt the patient to the respirator and facilitate blood flow to the heart.
Methods
High-frequency artificial ventilation is divided into three methods used by modern doctors:
- volumetric- characterized by a respiratory rate of 80-100 per minute;
- oscillatory– 600-3600 per minute with continuous or intermittent flow vibration;
- jet- 100-300 per minute, is the most popular, with it, oxygen or a mixture of gases under pressure is blown into the airways using a needle or a thin catheter, other options are an endotracheal tube, tracheostomy, a catheter through the nose or skin.
In addition to the considered methods, which differ in the frequency of breathing, ventilation modes are distinguished according to the type of apparatus used:
- Auto- the patient's breathing is completely suppressed by pharmacological preparations. The patient breathes completely with compression.
- Auxiliary- the person's breathing is preserved, and the gas is supplied when trying to take a breath.
- Periodic forced- used when transferring from mechanical ventilation to spontaneous breathing. A gradual decrease in the frequency of artificial breaths forces the patient to breathe on his own.
- With PEEP- with it, intrapulmonary pressure remains positive relative to atmospheric pressure. This allows you to better distribute air in the lungs, eliminate swelling.
- Diaphragm electrical stimulation- is carried out through external needle electrodes, which irritate the nerves on the diaphragm and cause it to contract rhythmically.

Ventilator
In the resuscitation mode or postoperative ward, a ventilator is used. This medical equipment is needed to supply a gas mixture of oxygen and dry air to the lungs. Forced mode is used to saturate cells and blood with oxygen and remove carbon dioxide from the body. How many types of ventilators:
- by type of equipment used- endotracheal tube, mask;
- according to the applied work algorithm- manual, mechanical, with neuro-controlled lung ventilation;
- according to the age- for children, adults, newborns;
- by drive– pneumomechanical, electronic, manual;
- by appointment- general, special;
- by applied field– intensive care unit, resuscitation, postoperative department, anesthesiology, newborns.
Technique for artificial lung ventilation
Doctors use ventilators to perform artificial ventilation. After examining the patient, the doctor sets the frequency and depth of breaths, selects the gas mixture. Gases for constant breathing are supplied through a hose connected to the endotracheal tube, the device regulates and controls the composition of the mixture. If a mask is used that covers the nose and mouth, the device is equipped with an alarm system that notifies of a violation of the breathing process. With prolonged ventilation, the endotracheal tube is inserted into the hole through the anterior wall of the trachea.
Problems during mechanical ventilation
After installing the ventilator and during its operation, problems may arise:
- The presence of the patient's struggle with the ventilator. For correction, hypoxia is eliminated, the position of the inserted endotracheal tube and the equipment itself are checked.
- Desynchronization with a respirator. Leads to a drop in tidal volume, inadequate ventilation. Causes are cough, breath holding, lung pathology, spasms in the bronchi, improperly installed apparatus.
- High airway pressure. The reasons are: violation of the integrity of the tube, bronchospasm, pulmonary edema, hypoxia.

Weaning from mechanical ventilation
The use of mechanical ventilation can be accompanied by injuries due to high blood pressure, pneumonia, decreased heart function, and other complications. Therefore, it is important to stop artificial ventilation as soon as possible, taking into account the clinical situation. The indication for weaning is the positive dynamics of recovery with indicators:
- restoration of breathing with a frequency of less than 35 per minute;
- minute ventilation decreased to 10 ml/kg or less;
- the patient does not have fever or infection, apnea;
- blood counts are stable.
Before weaning from the respirator, the remnants of muscle blockade are checked, and the dose of sedatives is reduced to a minimum. There are the following modes of weaning from artificial ventilation.
The fact that breathing air into the lungs can revive a person has been known since ancient times, but auxiliary devices for this began to be produced only in the Middle Ages. In 1530, Paracelsus first used a mouth air duct with leather bellows designed to fan a fire in a fireplace. After 13 years, Vezaleus published the work “On the structure of the human body”, in which he substantiated the benefits of ventilation through the tube inserted into the trachea. And in 2013, researchers at Case Western Reserve University created a prototype artificial lung. The device uses purified atmospheric air and does not need concentrated oxygen. The device is similar in structure to a human lung with silicone capillaries and alveoli and works on a mechanical pump. Biopolymer tubes mimic the branching of the bronchi into bronchioles. In the future, it is planned to improve the apparatus with reference to myocardial contractions. A mobile device is likely to replace a transport ventilator.
The dimensions of the artificial lung are up to 15x15x10 centimeters, they want to bring its dimensions as close as possible to the human organ. The huge area of the gas diffusion membrane gives a 3-5-fold increase in the efficiency of oxygen exchange.
While the device is being tested on pigs, tests have already shown its effectiveness in respiratory failure. The introduction of an artificial lung will help to abandon the more massive transport ventilators that work with explosive oxygen cylinders.
An artificial lung allows activation of a patient otherwise confined to a bed-mounted resuscitator or transport ventilator. And with activation, the chance for recovery and psychological state increase.
Patients awaiting a donor lung transplant usually have to stay in the hospital for quite a long time on an artificial oxygen machine, using which you can only lie in a bed and watch the machine breathe for you.
The project of an artificial lung capable of prosthetic respiratory failure gives these patients a chance for a speedy recovery.
The portable artificial lung kit includes the lung itself and a blood pump. Autonomous work is designed for up to three months. The small size of the device allows it to replace the transport ventilator of emergency medical services.
The work of the lung is based on a portable pump that enriches the blood with air gases.
Some people (especially newborns) do not need long-term high concentration oxygen because of its oxidizing properties.
Another non-standard analogue of mechanical ventilation used for high spinal cord injury is transcutaneous electrical stimulation of the phrenic nerves (“phrenicus stimulation”). A transpleural lung massage according to V.P. Smolnikov was developed - the creation of a state of pulsating pneumothorax in the pleural cavities.
Artificial lungs, compact enough to be carried in a regular backpack, have already been successfully tested on animals. Such devices can make the lives of those people whose own lungs do not function properly for any reason much more comfortable. Until now, very bulky equipment has been used for these purposes, but a new device being developed by scientists at the moment can change this once and for all.
A person whose lungs are unable to perform their main function, as a rule, join machines that pump their blood through a gas exchanger, enriching it with oxygen and removing carbon dioxide from it. Of course, during this process, a person is forced to lie on a bed or couch. And the longer they lie down, the weaker their muscles become, making recovery unlikely. It is in order to make patients mobile that compact artificial lungs have been developed. The problem became especially relevant in 2009, when there was an outbreak of swine flu, as a result of which many of the sick people lost their lungs.
Artificial lungs can not only help patients recover from certain lung infections, but also allow patients to wait for suitable donor lungs for transplantation. As you know, the queue can sometimes stretch for many years. The situation is complicated by the fact that in people with failed lungs, as a rule, the heart, which has to pump blood through, is also very weakened.
“Creating artificial lungs is a much more difficult task than designing an artificial heart. The heart simply pumps blood, while the lungs are a complex network of alvioli, within which the process of gas exchange takes place. To date, there is no technology that can even come close to the efficiency of real lungs, ”says William Federspiel of the University of Pittsburgh.
William Federspiel's team has developed an artificial lung that includes a pump (supporting the heart) and a gas exchanger, but the device is so compact that it can easily fit into a small bag or backpack. The device is connected to tubes connected to the human circulatory system, effectively enriching the blood with oxygen and removing excess carbon dioxide from it. This month, successful tests of the device on four experimental sheep were completed, during which the blood of animals was saturated with oxygen for different periods of time. Thus, scientists gradually brought the time of continuous operation of the device to five days.
An alternative model of artificial lungs is being developed by researchers at Carnegie Mellon University in Pittsburgh. This device is intended primarily for those patients whose heart is healthy enough to independently pump blood through an external artificial organ. The device is connected in the same way to tubes that are directly connected to the human heart, after which it is attached to the body with straps. So far, both devices need a source of oxygen, in other words, an additional portable cylinder. On the other hand, at the moment, scientists are trying to solve this problem, and they are quite successful.
Right now, researchers are testing a prototype artificial lung that no longer needs an oxygen tank. According to the official statement, the new generation of the device will be even more compact, and oxygen will be released from the surrounding air. The prototype is currently being tested on lab rats and is showing some truly impressive results. The secret of the new model of artificial lungs lies in the use of ultra-thin (only 20 micrometers) tubules made of polymer membranes, which significantly increase the gas exchange surface.
Modern medical technology allows you to replace completely or partially diseased human organs. An electronic heart pacemaker, a sound amplifier for people suffering from deafness, a lens made of special plastic - these are just some examples of the use of technology in medicine. Bioprostheses driven by miniature power supplies that respond to biocurrents in the human body are also becoming more widespread.
During the most complex operations performed on the heart, lungs or kidneys, invaluable assistance to physicians is provided by the “Artificial Circulatory Apparatus”, “Artificial Lung”, “Artificial Heart”, “Artificial Kidney”, which take on the functions of the operated organs, allow for a while to suspend their work.
"Artificial lung" is a pulsating pump that delivers air in portions at a frequency of 40-50 times per minute. An ordinary piston is not suitable for this: particles of the material of its rubbing parts or a seal can get into the air flow. Here and in other similar devices, corrugated metal or plastic bellows are used - bellows. Purified and brought to the required temperature, the air is supplied directly to the bronchi.
The “heart-lung machine” is similar. Its hoses are surgically connected to the blood vessels.
The first attempt to replace the function of the heart with a mechanical analogue was made as early as 1812. However, until now, among the many manufactured devices, there are no completely satisfying doctors.
Domestic scientists and designers have developed a number of models under the general name "Search". This is a four-chamber sac-type ventricular prosthesis designed for implantation in an orthotopic position.
The model distinguishes between the left and right halves, each of which consists of an artificial ventricle and an artificial atrium.
The constituent elements of the artificial ventricle are: body, working chamber, inlet and outlet valves. The ventricle housing is made of silicone rubber by layering. The matrix is immersed in a liquid polymer, removed and dried - and so on over and over again, until a multi-layer heart flesh is created on the surface of the matrix.
The working chamber is similar in shape to the body. It was made from latex rubber, and then from silicone. The design feature of the working chamber is a different wall thickness, in which active and passive sections are distinguished. The design is designed in such a way that even with full tension of the active sections, the opposite walls of the working surface of the chamber do not touch each other, which eliminates the injury of blood cells.
Russian designer Alexander Drobyshev, despite all the difficulties, continues to create new modern Poisk designs that will be much cheaper than foreign models.
One of the best foreign systems for today "Artificial heart" "Novacor" costs 400 thousand dollars. With her, you can wait at home for an operation for a whole year.
There are two plastic ventricles in the "Novakor" case. On a separate trolley there is an external service: a control computer, a control monitor, which remains in the clinic in front of the doctors. At home with the patient - a power supply, rechargeable batteries, which are replaced and recharged from the network. The task of the patient is to follow the green indicator of the lamps showing the charge of the batteries.
Devices "Artificial kidney" have been working for quite a long time and are successfully used by physicians.
Back in 1837, while studying the processes of movement of solutions through semipermeable membranes, T. Grechen was the first to use and put into use the term "dialysis" (from the Greek dialisis - separation). But only in 1912, on the basis of this method, an apparatus was constructed in the United States, with the help of which its authors carried out the removal of salicylates from the blood of animals in an experiment. In the device, which they called "artificial kidney", collodion tubes were used as a semi-permeable membrane, through which the animal's blood flowed, and outside they were washed with an isotonic sodium chloride solution. However, the collodion used by J. Abel turned out to be a rather fragile material, and later other authors tried other materials for dialysis, such as the intestines of birds, the swim bladder of fish, the peritoneum of calves, reed, and paper.
To prevent blood coagulation, hirudin, a polypeptide contained in the secretion of the salivary glands of a medicinal leech, was used. These two discoveries were the prototype for all subsequent developments in the field of extrarenal cleansing.
Whatever the improvements in this area, the principle remains the same. In any variant, the "artificial kidney" includes the following elements: a semi-permeable membrane, on one side of which blood flows, and on the other side - a saline solution. To prevent blood clotting, anticoagulants are used - medicinal substances that reduce blood clotting. In this case, the concentrations of low-molecular compounds of ions, urea, creatinine, glucose, and other substances with a small molecular weight are equalized. With an increase in the porosity of the membrane, the movement of substances with a higher molecular weight occurs. If we add to this process an excess hydrostatic pressure from the side of the blood or a negative pressure from the side of the washing solution, then the transfer process will be accompanied by the movement of water - convection mass transfer. Osmotic pressure can also be used to transfer water by adding osmotically active substances to the dialysate. Most often, glucose was used for this purpose, less often fructose and other sugars, and even more rarely products of other chemical origin. At the same time, by introducing glucose in large quantities, one can get a really pronounced dehydration effect, however, increasing the concentration of glucose in the dialysate above certain values is not recommended due to the possibility of complications.
Finally, it is possible to completely abandon the membrane-flushing solution (dialysate) and obtain an exit through the membrane of the liquid part of the blood: water and substances with a molecular weight of a wide range.
In 1925, J. Haas performed the first human dialysis, and in 1928 he also used heparin, since long-term use of hirudin was associated with toxic effects, and its very effect on blood coagulation was unstable. For the first time, heparin was used for dialysis in 1926 in an experiment by H. Nehels and R. Lim.
Since the materials listed above turned out to be of little use as a basis for creating semipermeable membranes, the search for other materials continued, and in 1938 cellophane was used for the first time for hemodialysis, which in subsequent years remained the main raw material for the production of semipermeable membranes for a long time.
The first “artificial kidney” device suitable for wide clinical use was created in 1943 by W. Kolff and H. Burke. Then these devices were improved. At the same time, the development of technical thought in this area at first concerned, to a greater extent, the modification of dialyzers, and only in recent years began to affect the devices themselves to a large extent.
As a result, two main types of dialyzer appeared, the so-called coil dialyzer, where cellophane tubes were used, and plane-parallel, in which flat membranes were used.
In 1960, F. Keel designed a very successful version of a plane-parallel dialyzer with polypropylene plates, and over the course of a number of years this type of dialyzer and its modifications spread throughout the world, taking a leading place among all other types of dialyzers.
Then the process of creating more efficient hemodialyzers and simplifying the technique of hemodialysis developed in two main directions: the design of the dialyzer itself, with single-use dialyzers taking the dominant position over time, and the use of new materials as a semipermeable membrane.
The dialyzer is the heart of the "artificial kidney", and therefore the main efforts of chemists and engineers have always been aimed at improving this particular link in the complex system of the apparatus as a whole. However, technical thought did not disregard the apparatus as such.
In the 1960s, the idea arose to use the so-called central systems, that is, “artificial kidney” devices, in which dialysate was prepared from a concentrate - a mixture of salts, the concentration of which was 30-34 times higher than their concentration in the patient's blood.
A combination of flush dialysis and recirculation techniques has been used in a number of artificial kidney machines, such as by the American firm Travenol. In this case, about 8 liters of dialysate circulated at high speed in a separate container in which the dialyzer was placed and into which 250 milliliters of fresh solution was added every minute and the same amount was thrown into the sewer.
At first, simple tap water was used for hemodialysis, then, due to its contamination, in particular with microorganisms, they tried to use distilled water, but this turned out to be very expensive and inefficient. The issue was radically resolved after the creation of special systems for the preparation of tap water, which includes filters for its purification from mechanical impurities, iron and its oxides, silicon and other elements, ion-exchange resins to eliminate water hardness and installations of the so-called "reverse" osmosis.
Much effort has been expended on improving the monitoring systems of artificial kidney devices. So, in addition to constantly monitoring the temperature of the dialysate, they began to constantly monitor with the help of special sensors the chemical composition of the dialysate, focusing on the overall electrical conductivity of the dialysate, which changes with a decrease in salt concentration and increases with an increase in it.
After that, ion-selective flow sensors began to be used in “artificial kidney” devices, which would constantly monitor the ion concentration. The computer, on the other hand, made it possible to control the process by introducing the missing elements from additional containers, or to change their ratio using the feedback principle.
The value of ultrafiltration during dialysis depends not only on the quality of the membrane, in all cases the transmembrane pressure is the decisive factor, therefore pressure sensors have become widely used in monitors: the degree of dilution in dialysate, the pressure value at the inlet and outlet of the dialyzer. Modern technology using computers makes it possible to program the ultrafiltration process.
Leaving the dialyzer, the blood enters the patient's vein through an air trap, which makes it possible to judge by eye the approximate amount of blood flow, the tendency of blood to clot. To prevent air embolism, these traps are equipped with air ducts, with the help of which they regulate the level of blood in them. Currently, in many devices, ultrasonic or photoelectric detectors are put on air traps, which automatically block the venous line when the blood level in the trap falls below a predetermined level.
Recently, scientists have created devices that help people who have lost their sight - completely or partially.
Miracle glasses, for example, were developed by the research and development manufacturing company "Rehabilitation" on the basis of technologies that were previously used only in military affairs. Like a night sight, the device operates on the principle of infrared location. The matte black lenses of the glasses are actually Plexiglas plates, between which a miniature location device is enclosed. The entire locator, together with the spectacle frame, weighs about 50 grams - about the same as ordinary glasses. And they are selected, like glasses for the sighted, strictly individually, so that it is both convenient and beautiful. "Lenses" not only perform their direct functions, but also cover eye defects. Of the two dozen options, everyone can choose the most suitable for themselves.
Using glasses is not difficult at all: you need to put them on and turn on the power. The source of energy for them is a flat battery the size of a cigarette pack. Here, in the block, the generator is also placed.
The signals emitted by it, having come across an obstacle, come back and are caught by the "receiver lenses". The received impulses are amplified, compared with the threshold signal, and if there is an obstacle, the buzzer immediately sounds - the louder the closer the person came to it. The range of the device can be adjusted using one of two ranges.
Work on the creation of an electronic retina is being successfully carried out by American specialists from NASA and the Main Center at Johns Hopkins University.
At first, they tried to help people who still had some remnants of vision. “Teleglasses have been created for them,” S. Grigoriev and E. Rogov write in the journal “Young Technician”, “where miniature television screens are installed instead of lenses. Equally tiny video cameras, located on the frame, send into the image everything that falls into the field of view of an ordinary person. However, for the visually impaired, the picture is also decrypted using the built-in computer. Such a device does not create special miracles and does not make the blind sighted, experts say, but it will allow the maximum use of the visual abilities that a person still has, and facilitate orientation.
For example, if a person has at least part of the retina left, the computer will “split” the image in such a way that a person can see the environment, at least with the help of the preserved peripheral areas.
According to the developers, such systems will help approximately 2.5 million people suffering from visual impairments. But what about those whose retina is almost completely lost? For them, scientists from the eye center at Duke University (North Carolina) are mastering the operation of implanting an electronic retina. Special electrodes are implanted under the skin, which, when connected to nerves, transmit an image to the brain. The blind sees a picture consisting of individual luminous dots, very similar to the display board that is installed in stadiums, train stations and airports. The image on the "scoreboard" is again created by miniature television cameras mounted on a spectacle frame.
And, finally, the last word of science today is an attempt to create new sensitive centers on the damaged retina using the methods of modern microtechnology. Prof. Rost Propet and his colleagues are now engaged in such operations in North Carolina. Together with NASA specialists, they created the first samples of subelectronic retina, which is directly implanted in the eye.
“Our patients, of course, will never be able to admire the paintings of Rembrandt,” comments the professor. “However, they will still be able to distinguish where the door is and where the window is, road signs and signboards…”
100 great wonders of technology
St. Petersburg State Polytechnic University
COURSE WORK
Discipline: Medical Application Materials
Topic: artificial lung
St. Petersburg
List of symbols, terms and abbreviations 3
1. Introduction. four
2. Anatomy of the human respiratory system.
2.1. Airways. four
2.2. Lungs. 5
2.3. Pulmonary ventilation. 5
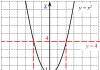
2.4. Changes in lung volume. 6
3. Artificial lung ventilation. 6
3.1. Basic methods of artificial lung ventilation. 7
3.2. Indications for the use of artificial lung ventilation. eight
3.3. Control of the adequacy of artificial lung ventilation.
3.4. Complications with artificial ventilation of the lungs. 9
3.5. Quantitative characteristics of the modes of artificial lung ventilation. ten
4. Artificial lung ventilation apparatus. ten
4.1. The principle of operation of the artificial lung ventilation apparatus. ten
4.2. Medical and technical requirements for the ventilator. eleven
4.3. Schemes for supplying a gas mixture to a patient.
5. Heart-lung machine. 13
5.1. Membrane oxygenators. fourteen
5.2. Indications for extracorporeal membrane oxygenation. 17
5.3. Cannulation for extracorporeal membrane oxygenation. 17
6. Conclusion. eighteen
List of used literature.
List of symbols, terms and abbreviations
IVL - artificial lung ventilation.
BP - blood pressure.
PEEP is positive end-expiratory pressure.
AIC - heart-lung machine.
ECMO - extracorporeal membrane oxygenation.
VVEKMO - venovenous extracorporeal membrane oxygenation.
VAECMO - veno-arterial extracorporeal membrane oxygenation.
Hypovolemia is a decrease in the volume of circulating blood.
This usually refers more specifically to a decrease in plasma volume.
Hypoxemia is a decrease in the oxygen content in the blood as a result of circulatory disorders, increased tissue demand for oxygen, a decrease in gas exchange in the lungs during their diseases, a decrease in the hemoglobin content in the blood, etc.
Hypercapnia is an increased partial pressure (and content) of CO2 in arterial blood (and in the body).
Intubation is the introduction of a special tube into the larynx through the mouth in order to eliminate respiratory failure in case of burns, some injuries, severe spasms of the larynx, laryngeal diphtheria and its acute, quickly resolved edema, for example, allergic.
A tracheostomy is an artificially formed fistula of the trachea, brought into the outer region of the neck, for breathing, bypassing the nasopharynx.
A tracheostomy cannula is inserted into the tracheostomy.
Pneumothorax is a condition characterized by the accumulation of air or gas in the pleural cavity.
1. Introduction.
The human respiratory system provides in-stu-p-le-tion into the body of ki-slo-ro-yes and removal of coal-le-ki-slo-go gas. Transport of gases and other non-ho-di-my or-ha-low-mu substances os-sche-st-v-la-et-sya with the help of cro- ve-nos-noy sis-the-we.
The function of the respiratory-ha-tel-noy system-te-we comes down only to supplying the blood with a dos-that-precise amount of ki -slo-ro-yes and remove carbon-le-sour gas from it. Hi-mi-che-recovery-sta-new-le-nie mo-le-ku-lyar-no-go ki-slo-ro-yes with ob-ra-zo-va-ni-em water-du - lives for mammals, the main sources of energy. Without it, life cannot continue for more than a few seconds.
Res-sta-nov-le-niu ki-slo-ro-yes co-put-st-vu-et about-ra-zo-va-ing CO2.
The ki-slo-genus included in CO2 does not pro-is-ho-dit not-in-medium-st-ven-but from the mo-le-ku-lar-no-go ki-slo-genus. The use of O2 and the formation of CO2 are connected with me-zh-du with-battle pro-me-zhu-precise-we-mi me-ta-bo -li-che-ski-mi re-ak-tion-mi; theo-re-ti-che-ski each of them lasts for some time.
The exchange of O2 and CO2 between the or-ha-low-mom and the environment on-zy-va-et-sya dy-ha-ni-em. In higher animals, the process of breathing-ha-niya osu-sche-st-in-la-et-sya bla-go-da-rya row-du-after-to-va-tel- nyh processes.
1. The exchange of gases between the medium and the lungs, which is usually referred to as "easy ven-ti-la-tion."
Exchange of gas-call between al-ve-o-la-mi lungs and blood-view (easy breathing).
3. Exchange of gases between blood-view and tissue. Gases re-re-ho-dyat inside the fabric to the places of demand (for O2) and from the places of production (for CO2) (glue- accurate breathing).
You-pa-de-any of any of these processes bring-in-dit to na-ru-she-ni-pits of dy-ha-nia and creates a danger to life - not a person.
2.
Ana-to-miya of the human respiratory system.
Dy-ha-tel-naya sys-te-ma che-lo-ve-ka is composed of tissues and or-ga-nov, providing-ne-chi-vayu-schih le-goch-nuyu veins -ti-la-tion and easy breathing. To the air-du-ho-nos-ny ways from-no-syat-sya: nose, in-lost of the nose, but-with-swallow-ka, gore-tan, tra-cheya, bron-hi and bron-chio-ly.
Lungs consist of bron-chi-ol and al-ve-o-lyar-nyh bags, as well as ar-te-riy, ka-pil-la-ditch and veins le-goch-no-go kru-ha kro-in-o-ra-sche-niya. To the element-men-there ko-st-but-we-shchech-noy system-the-we, connected with the breath-ha-ni-em, from-no-syat-sya rib-ra, inter- rib muscles, diaphragm and auxiliary respiratory muscles.
Air-du-ho-nose-nye way.
The nose and the cavity of the nose serve as a pro-in-dia-schi-mi ka-na-la-mi for air-du-ha, in some it is on-gre-va-et-sya , uv-lazh-nya-et-sya and filter-ru-et-sya. In-lost but-sa you-stall-on-bo-ha-you-ku-la-ri-zo-van-noy mu-zi-stay shell-coy. Many-number-len-same-st-hair-los-ki, as well as supplied-wife res-nich-ka-mi epi-te-li-al-nye and bo-ka- lo-vid-nye cells serve for the eyes of the breath-hae-mo-th air-du-ha from solid particles.
In the upper part of the los-ti lie ob-nya-tel-cells.
Gor-tan lies between tra-he-she and the root of the tongue. In-the-lost of the mountains-ta-not once-de-le-on-two warehouses-ka-mi sli-zi-stand shell-ki, not half-no-stu converge-dya-schi-mi-sya on middle line. Pro-country-st-in-between these warehouses-ka-mi - go-lo-so-vaya gap for-schi-sche-but plate-coy in-lok-no-hundred-go cartilage - above-mountain-tan-no-com.
Tra-heya na-chi-na-et-sya at the lower end of the mountains-ta-ni and descends into the chest cavity, where de-lit-sya on the right -vy and left bronchi; wall-ka its about-ra-zo-va-on with-one-ni-tel-noy tissue and cartilage.
Hours, attached to pi-che-vo-du, for-me-shche-we-fibrous ligament. The right bronchus is usually short-ro-che and wide-re left-of-the-go. Enter into the lungs, the main bronchi in degrees, but de-lyat into more and more small tubes (bron-chio-ly), the most small some of some of them are ko-nech-nye bron-chio-ly yav-la-yut-sya in the next element of the air-du-ho-nos-ny ways. From the mountains-ta-ni to the end of the bron-chi-ol pipes you-stlay-we-me-tsa-tel-ny epi-the-li-em.
2.2.
In general, the lungs have the appearance of lips-cha-tyh, in-fig-tyh-well-with-vid-nyh-ra-zo-va-ny, lying in both of them in-lo-vi-nah chest-noy in-los-ti. The smallest structural element of the easy-to-go - dol-ka consists of a finite bron-chio-la, leading to the leg-goch-nu bron-hyo-lu and al-ve-o-lar-ny bag. The walls of the light bron-chio-ly and al-ve-o-lyar-no-go bag ob-ra-zu-yut corner-lub-le-nia - al-ve-o-ly . This structure of the lungs increases their respiratory surface, which is 50-100 times the surface of the body.
The walls of al-ve-ol consist of one layer of epi-te-li-al-nyh cells and ok-ru-zhe-ny le-goch-ny-mi ka-pil -la-ra-mi. The inner-ren-nya-top-ness of al-ve-o-ly in-roof-ta-top-but-st-but-active-thing-th-st-vom sur-fak-tan- volume. From-del-naya al-ve-o-la, closely co-at-ka-say-scha-sya with co-sed-ni-mi structures-tu-ra-mi, has no form -right-vil-no-go-many-grand-no-ka and approximate sizes up to 250 microns.
It’s supposed to be considered that the general surface is al-ve-ol, through some os-shche-st-in-la-et-sya gas-zo-ob -men, ex-po-nen-qi-al-but for-wee-sit from weight te-la. With age, from-me-cha-et-sya, a decrease in the area-di-top-no-sti al-ve-ol.
Each one is light-something ok-ru-same-but bag-com - a spit-swarm. The outer (pa-ri-tal-ny) sheet of the pleura is attached to the inner-ren-it on the top of the chest wall and the diaphragm -me, internal-ren-ny (vis-ce-ral-ny) in-roof-va-et easy.
The gap between me-zh-du-li-st-ka-mi on-zy-va-et-sya spleen-ral-noy-lo-stu. With the movement of the chest, the inner leaf usually slides easily along the outside. The pressure in the plevis-ral-noy in-los-ti is always less than at-mo-spheres-no-go (from-ri-tsa-tel-noe).
Artificial organs: a person can do everything
In the conditions-lo-vi-yah, the intra-pleural pressure of a person is on average 4.5 Torr below the at-mo-spheres -no-go (-4.5 Torr). Inter-pleural-noe pro-country-st-in-f-du l-ki-mi on-zy-va-et-s-mid-to-ste-ni-em; there is a tra-hea in it, a goiter is the same-le-za (ti-mus) and a heart with pain-shi-mi so-su-da-mi, lim-fa-ti- che knots and pi-shche-water.
The light art-the-riya does not draw blood from the right-of-the-well-daughter of the heart, it is divided into the right and left branches, which -something on the right-la-ut-Xia to the lungs.
These ar-te-rii vet-vyat-sya, following the bron-ha-mi, supply large structures-tu-ry easily and form pil-la-ry, op-le-melting walls-ki al-ve-ol. Air-spirit in al-ve-o-le from-de-len from cro-vie in cap-pil-la-re wall-coy al-ve-o-ly, wall-coy cap-pil-la-ra and in some cases, pro-me-zhu-accurate layer between me-zh-du-no-mi.
From the ka-pil-la-ditch, the blood flows into small veins, some of them at the end of the ends unite and form zu-yut pulmonary veins, supplying blood to the left pre-heart.
Bron-chi-al-nye ar-te-rii of a pain-sho-th circle also bring blood to the lungs, but they supply bron-chi and bron-chio -ly, lim-fa-ti-che-knots, walls of cro-ve-nos-nyh co-courts and pleu-ru.
Most of this blood is from-te-ka-et to the bron-chi-al-veins, and from-to-yes - to the non-pair (on the right) and in the lu -not-pair-nuyu (left-va). Very not-pain-shoe-whether-che-st-vo ar-te-ri-al-noy bron-hi-al-noy blood-vi-st-pa-et in l-goch-ny ve-ns .
10 artificial organs to create a real person
Orchestrion(German Orchestrion) - the name of a number of musical instruments, the principle of which is similar to the organ and harmonica.
The orchestrion was originally a portable organ designed by Abbot Vogler in 1790. It contained about 900 pipes, 4 manuals with 63 keys each and 39 pedals. The “revolutionary” nature of Vogler's orchestra consisted in the active use of combination tones, which made it possible to significantly reduce the size of the labial organ pipes.
In 1791, the same name was given to an instrument created by Thomas Anton Kunz in Prague. This instrument was equipped with both organ pipes and piano-like strings. Kunz's orchestra had 2 manuals of 65 keys and 25 pedals, had 21 registers, 230 strings and 360 pipes.
At the beginning of the 19th century, under the name orchestrion (also orchestra) a number of automatic mechanical instruments appeared, adapted to imitate the sound of an orchestra.
The tool looked like a cabinet, inside of which a spring or pneumatic mechanism was placed, which, when a coin was thrown, was activated. The arrangement of the strings or pipes of the instrument was chosen in such a way that certain musical works sounded during the operation of the mechanism. The instrument gained particular popularity in the 1920s in Germany.
Later, the orchestrion was supplanted by gramophone record players.
see also
Notes
Literature
- Orchestra // Musical Instruments: Encyclopedia. - M.: Deka-VS, 2008. - S. 428-429. - 786 p.
- Orchestra // Great Russian Encyclopedia. Volume 24. - M., 2014. - S. 421.
- Mirek A.M. Vogler's orchestra // Reference to the harmonic scheme. - M.: Alfred Mirek, 1992. - S. 4-5. - 60 s.
- Orchestra // Musical Encyclopedic Dictionary. - M.: Soviet Encyclopedia, 1990. - S. 401. - 672 p.
- Orchestra // Musical Encyclopedia. - M.: Soviet Encyclopedia, 1978. - T. 4. - S. 98-99. - 976 p.
- Herbert Jüttemann: Orchestrien aus dem Schwarzwald: Instrumente, Firmen und Fertigungsprogramme.
Bergkirchen: 2004. ISBN 3-932275-84-5.
CC © wikiredia.ru
The experiment carried out at the University of Granada was the first in which an artificial skin was created with a dermis based on an aragoso-fibrin biomaterial. Until now, other biomaterials such as collagen, fibrin, polyglycolic acid, chitosan, etc. have been used.
A more stable skin has been created with functionality similar to that of normal human skin.
artificial intestine
In 2006, British scientists announced the creation of an artificial intestine capable of accurately reproducing the physical and chemical reactions that occur during digestion.
The organ is made of special plastic and metal, which do not collapse or corrode.
Then, for the first time in history, work was done that demonstrated how human pluripotent stem cells in a petri dish can be assembled into body tissue with a three-dimensional architecture and the type of connections inherent in naturally developed flesh.
Artificial intestinal tissue could be the #1 therapeutic option for people suffering from necrotizing enterocolitis, inflammatory bowel disease, and short bowel syndrome.
During the research, a group of scientists led by Dr. James Wells used two types of pluripotent cells: embryonic human stem cells and induced, obtained by reprogramming human skin cells.
Embryonic cells are called pluripotent because they are able to transform into any of the 200 different types of cells in the human body.
The induced cells are suitable for "combing" the genotype of a particular donor, without the risk of further rejection and associated complications. This is a new invention of science, so it is not yet clear whether the induced cells of the adult organism have the same potential as the cells of the embryo.
The artificial intestinal tissue was "released" in two forms, assembled from two different types of stem cells.
It took a lot of time and effort to turn individual cells into intestinal tissue.
The scientists harvested tissue using chemicals as well as proteins called growth factors. In a test tube, living matter grew in the same way as in a developing human embryo.
artificial organs
First, the so-called endoderm is obtained, from which the esophagus, stomach, intestines and lungs grow, as well as the pancreas and liver. But doctors gave the command to the endoderm to develop only into the primary cells of the intestine. It took 28 days for them to grow to tangible results. The tissue has matured and acquired the absorptive and secretory functionality of a healthy human digestive tract. It also has specific stem cells, which will now be much easier to work with.
artificial blood
There is always a shortage of blood donors - Russian clinics are provided with blood products for only 40% of the norm.
One heart operation using the artificial circulation system requires the blood of 10 donors. There is a possibility that artificial blood will help solve the problem - as a constructor, scientists have already begun to collect it. Synthetic plasma, erythrocytes and platelets have been created. A little more, and we can become Terminators!
Plasma- one of the main components of blood, its liquid part. "Plastic plasma", created at the University of Sheffield (Great Britain), can perform all the functions of a real one and is absolutely safe for the body. It contains chemicals that can carry oxygen and nutrients. Today, artificial plasma is designed to save lives in extreme situations, but in the near future it will be used everywhere.
Well, that's impressive. Although it’s a little scary to imagine that liquid plastic is flowing inside you, or rather, plastic plasma. After all, to become blood, it still needs to be filled with erythrocytes, leukocytes, and platelets. Specialists from the University of California (USA) decided to help their British colleagues with the "bloody constructor".
They developed fully synthetic erythrocytes from polymers capable of carrying oxygen and nutrients from the lungs to organs and tissues and vice versa, that is, to perform the main function of real red blood cells.
In addition, they can deliver drugs to cells. Scientists are confident that in the coming years, all clinical trials of artificial erythrocytes will be completed, and they can be used for transfusion.
True, having previously diluted them in plasma - even in natural, even in synthetic.
Not wanting to lag behind their California counterparts, artificial platelets developed by scientists from Case Western Reserve University, Ohio. To be precise, these are not exactly platelets, but their synthetic assistants, also consisting of a polymeric material. Their main task is to create an effective environment for gluing platelets, which is necessary to stop bleeding.
Now in clinics, platelet mass is used for this, but obtaining it is a painstaking and rather long process. It is necessary to find donors, to make a strict selection of platelets, which, moreover, are stored for no more than 5 days and are susceptible to bacterial infections.
The advent of artificial platelets removes all these problems. So the invention will be a good helper and will allow doctors not to be afraid of bleeding.
Real & artificial blood. What's better?
The term "artificial blood" is a bit of a misnomer. Real blood performs a large number of tasks. Artificial blood can only perform some of them so far. If a full-fledged artificial blood is created that can completely replace the real one, this will be a real breakthrough in medicine.
Artificial blood has two main functions:
1) increases the volume of blood cells
2) performs the functions of oxygen enrichment.
While a substance that increases the volume of blood cells has long been used in hospitals, oxygen therapy is still under development and clinical research.
3. Alleged advantages and disadvantages of artificial blood
artificial bones
Physicians at Imperial College London claim they have succeeded in producing a pseudo-bone material that is most similar in composition to real bones and has minimal chance of rejection.
New artificial bone materials actually consist of three chemical compounds at once, which simulate the work of real bone tissue cells.
Doctors and specialists in prosthetics around the world are now developing new materials that could serve as a complete replacement for bone tissue in the human body.
However, to date, scientists have created only bone-like materials, which have not yet been transplanted instead of real bones, albeit broken ones.
The main problem with such pseudo-bone materials is that the body does not recognize them as “native” bone tissues and does not take root to them. As a result, large-scale rejection processes can begin in the body of a patient with transplanted bones, which, in the worst case scenario, can even lead to a massive failure in the immune system and death of the patient.
artificial lung
American scientists from Yale University, led by Laura Niklason, have made a breakthrough: they managed to create an artificial lung and transplant it into rats.
Also, a lung was created separately that works autonomously and imitates the work of a real organ.
It must be said that the human lung is a complex mechanism.
The surface area of one lung in an adult human is about 70 square meters, assembled so as to ensure the efficient transfer of oxygen and carbon dioxide between blood and air. But lung tissue is difficult to repair, so at the moment, the only way to replace damaged parts of the organ is with a transplant. This procedure is very risky due to the high percentage of rejections.
According to statistics, ten years after transplantation, only 10-20% of patients remain alive.
"Artificial lung" is a pulsating pump that delivers air in portions at a frequency of 40-50 times per minute. A conventional piston is not suitable for this; particles of the material of its rubbing parts or a seal can get into the air flow. Here, and in other similar devices, corrugated metal or plastic bellows are used - bellows.
Purified and brought to the required temperature, the air is supplied directly to the bronchi.
Change hand? No problem!..
artificial hands
Artificial hands in the 19th century
were divided into "working hands" and "cosmetic hands", or luxury goods.
For a bricklayer or laborer, they were limited to imposing on the forearm or shoulder a bandage made of a leather sleeve with fittings, to which a tool corresponding to the worker's profession was attached - tongs, a ring, a hook, etc.
Cosmetic artificial hands, depending on occupation, lifestyle, degree of education and other conditions, were more or less complex.
The artificial hand could be in the form of a natural one, wearing an elegant kid glove, capable of producing fine work; write and even shuffle cards (like the famous hand of General Davydov).
If the amputation did not reach the elbow joint, then with the help of an artificial arm it was possible to return the function of the upper limb; but if the upper arm was amputated, then the work of the hand was possible only through the medium of voluminous, very complex and demanding apparatuses.
In addition to the latter, the artificial upper limbs consisted of two leather or metal sleeves for the upper arm and forearm, which were movably hinged above the elbow joint by means of metal splints. The hand was made of light wood and either fixed to the forearm or movable.
There were springs in the joints of each finger; from the ends of the fingers go intestinal strings, which were connected behind the wrist joint and continued in the form of two stronger laces, and one, passing through the rollers through the elbow joint, was attached to the spring on the upper shoulder, while the other, also moving on the block, freely ended with an eye.
With voluntary flexion of the elbow joint, the fingers closed in this apparatus and completely closed if the shoulder was bent at a right angle.
For orders of artificial hands, it was enough to indicate the measures of the length and volume of the stump, as well as the healthy hand, and explain the technique of the purpose that they should serve.
Prostheses for hands should have all the necessary properties, for example, the function of closing and opening the hand, holding and releasing anything from the hands, and the prosthesis should have a look that replicates the lost limb as closely as possible.
There are active and passive prosthetic hands.
Passive ones only copy the appearance of the hand, while active ones, which are divided into bioelectric and mechanical ones, perform much more functions. The mechanical hand replicates a real hand quite accurately, so that any amputee can relax among people, and can also pick up an object and release it.
The bandage, which is attached to the shoulder girdle, sets the brush in motion.
The bioelectric prosthesis works thanks to electrodes that read the current generated by the muscles during contraction, the signal is transmitted to the microprocessor and the prosthesis moves.
artificial legs
For a person with physical damage to the lower extremities, of course, high-quality leg prostheses are important.
It is on the level of amputation of the limb that the correct choice of the prosthesis will depend, which will replace and even be able to restore many of the functions that were characteristic of the limb.
There are prostheses for people, both young and old, as well as for children, athletes, and those who, despite amputation, lead an equally active life. A high-class prosthesis consists of a foot system, knee joints, adapters made of high-class material and increased strength.
Pages:← previous1234next →
Severe respiratory disorders require emergency assistance in the form of forced ventilation. Whether the failure of the lungs themselves or the respiratory muscles is an unconditional need to connect complex equipment to saturate the blood with oxygen. Various models of ventilators are an essential equipment of intensive care or resuscitation services necessary to maintain the life of patients who have manifested acute respiratory disorders.
In emergency situations, such equipment, of course, is important and necessary. However, as a means of regular and long-term therapy, it, unfortunately, is not without drawbacks. For example:
- the need for a permanent stay in the hospital;
- permanent risk of inflammatory complications due to the use of a pump to supply air to the lungs;
- restrictions on the quality of life and independence (immobility, inability to eat normally, speech difficulties, etc.).
To eliminate all these difficulties, while simultaneously improving the process of blood oxygen saturation, the innovative artificial lung system iLA allows resuscitation, therapeutic and rehabilitation use of which is offered today by German clinics.
Risk-free coping with respiratory distress
The iLA system is a fundamentally different development. Its action is extrapulmonary and completely non-invasive. Respiratory disorders are overcome without forced ventilation. The scheme of blood oxygen saturation is characterized by the following promising innovations:
- lack of an air pump;
- absence of invasive ("embedded") devices in the lungs and airways.
Patients who have an artificial lung iLA are not tied to a stationary device and a hospital bed, they can move normally, communicate with other people, eat and drink on their own.
The most important advantage: there is no need to introduce a patient into an artificial coma with artificial respiratory support. The use of standard ventilators in many cases requires a comatose "shutdown" of the patient. For what? To alleviate the physiological consequences of respiratory depression of the lungs. Unfortunately, it is a fact: ventilators depress the lungs. The pump delivers air under pressure. The rhythm of air supply reproduces the rhythm of breaths. But on a natural breath, the lungs expand, as a result of which the pressure in them decreases. And at the artificial inlet (forced air supply), the pressure, on the contrary, increases. This is the oppression factor: the lungs are in a stress mode, which causes an inflammatory reaction, which in especially severe cases can be transmitted to other organs - for example, the liver or kidneys.
This is why two factors are of paramount and equal importance in the use of pumped respiratory support devices: urgency and caution.
The iLA system, by expanding the range of benefits in artificial respiratory support, eliminates the associated dangers.
How does a blood oxygenator work?
The name "artificial lung" has a special meaning in this case, since the iLA system operates completely autonomously and is not a functional addition to the patient's own lungs. In fact, this is the world's first artificial lung in the true sense of the word (and not a pulmonary pump). It is not the lungs that are ventilated, but the blood itself. A membrane system was used to saturate the blood with oxygen and remove carbon dioxide. By the way, in German clinics, the system is called so: a membrane ventilator (iLA Membranventilator). Blood is supplied to the system in a natural order, by the force of compression of the heart muscle (and not by a membrane pump, as in a heart-lung machine). Gas exchange is carried out in the membrane layers of the apparatus in much the same way as in the alveoli of the lungs. The system really works as a “third lung”, unloading the sick respiratory organs of the patient.
The membrane exchange apparatus (the "artificial lung" itself) is compact, its dimensions are 14 by 14 centimeters. The patient carries the instrument with him. Blood enters it through a catheter port, a special connection to the femoral artery. To connect the device, no surgical operation is required: the port is inserted into the artery in much the same way as a syringe needle. The connection is made in the inguinal zone, the special design of the port does not restrict mobility and does not cause any inconvenience to the patient at all.
The system can be used without interruption for quite a long time, up to one month.
Indications for iLA use
In principle, these are any respiratory disorders, especially chronic ones. To the greatest extent, the advantages of an artificial lung are manifested in the following cases:
- chronic obstructive pulmonary disease;
- acute respiratory distress syndrome;
- respiratory injuries;
- the so-called Weaning phase: weaning from the ventilator;
- patient support before lung transplantation.