An overactive bladder (OAB) is a combination of symptoms caused by spontaneous contraction of the bladder muscles when urine accumulates. These signs include:
- desire to empty the bladder at night;
- uncontrollable urges, which can lead to urinary incontinence.
There are two types of hyperactivity: idiopathic (without a clear cause), occurring in about 65% of patients, and neurogenic (caused by diseases of the nervous system, and so on), observed in about 24% of patients. Urologists also distinguish a form in which all of the listed symptoms occur in the absence of hyperactivity of the bladder muscle itself (detrusor), which accounts for 11% of all cases of OAB. The latter form occurs in women much more often than in men.
Prevalence
Approximately one in five adults on Earth has the disease. Women suffer somewhat more often than men, especially with some forms of the disease. OAB occurs in 16% of women in Russia. However, the myth that OAB is a disease exclusively of women is associated with a much rarer appeal of men to a doctor about this. The greatest number of patients falls ill at the age of about 40 years, and over the next 20 years, the incidence among the female population is higher. Among patients over the age of 60, the number of men is gradually increasing.
The incidence of this disease is comparable to morbidity or depression, that is, it is a fairly widespread chronic disease. A feature of the disease is that even in the United States of America, 70% of patients for some reason do not receive treatment.
This is largely due to the embarrassment of patients and poor awareness of the possibility of treating this disease. Therefore, patients adapt by changing their usual way of life, while its quality is significantly reduced. It becomes impossible to travel long distances or even a simple shopping trip or excursion. Night sleep is disturbed. Patients are less likely to meet with relatives and friends. Their work in a team is disrupted. All this leads to a violation of the social adaptation of patients with OAB, making this disease a significant medical and social problem.
It should be noted the low awareness of not only patients, but also doctors in matters related to the causes, manifestations, diagnosis and treatment of the disease.
Causes
As the name suggests, idiopathic hyperactivity has an unexplained cause. It is believed that damage to the nerve endings responsible for the functioning of the bladder muscle, as well as changes in the structure of this muscle, are involved in its development. In places where the innervation of the muscle is disturbed, there is an increased excitability of muscle cells adjacent to each other. At the same time, the reflex contraction of the muscle cell, provoked by the expansion of the bladder during its filling, is transmitted like a chain reaction along the entire wall of the organ. This theory, which explains the development of hyperactivity by an excessive contractile response of cells during denervation (lack of normal nervous regulation), is generally accepted.
Factors contributing to the development of OAB:
- female;
- old age (60 years or more);
- irritable bowel syndrome;
- depression, emotional instability, chronic nervous tension.
The predisposition of women to the development of the disease is due, as experts today believe, to a lower level of serotonin in their brain. It is further reduced during any hormonal changes, making the woman more likely to fall prey to the disease initially.
In elderly patients, the tendency to the appearance of OAB is due to a decrease in the elasticity of the bladder muscle and its ischemia, that is, insufficient blood supply. These factors lead to the death of muscle cells and damage to the nerves responsible for the correct rhythm of urination. This also starts a chain reaction of muscle cells associated with denervation of the bladder muscle.
Another provoking factor, characteristic mainly for women, is the inflammatory processes of the genitourinary tract.
Neurogenic hyperactivity occurs in people of both sexes with the same frequency. It is caused by damage to the pathways that conduct nerve impulses through the spinal cord and the overlying nerve centers. At the same time, the brain affected as a result of the disease gives signals for emptying when the bladder is not full, causing the classic OAB clinic. Neurogenic hyperactivity occurs with brain tumors, severe, Parkinson's disease, injuries and and the spinal cord.
External manifestations
There are three main symptoms of OAB:
- urination more than 8 times a day (of which more than once at night);
- urgent (urgent), sudden and very strong urges at least twice a day;
- urinary incontinence.
The most persistent symptom is frequent urination, which sometimes makes patients completely unable to work and leads to rash decisions with dire consequences.
Urinary incontinence is more rare, but it is even more difficult to tolerate. Within three years, in about a third of patients, this symptom either disappears on its own without treatment, then reappears.
Diagnostics

Complaints, the history of life and illness of the patient are studied. The patient is asked to keep a urinary diary for at least three days. It will be a great time saver if the patient gets to the initial appointment with the urologist with an already filled diary.
The diary should record the time of urination and the amount of urine excreted. Very useful additional information:
- the presence of imperative (“ordering”) urges;
- episodes of incontinence;
- the use of special gaskets and their number;
- the amount of fluid you drink per day.
When collecting an anamnesis, special attention is paid to neurological and gynecological diseases, as well as diabetes mellitus. Be sure to clarify information about childbirth and surgical interventions on the muscles of the perineum.
A vaginal examination and a cough test are performed (during such an examination, the woman is asked to cough). Conduct an ultrasound examination of the uterus, kidneys, bladder. They take a urine sample and do a culture to check for infection. The patient should be examined by a neurologist and given a detailed conclusion.
Urodynamic studies were previously considered an integral part of the diagnosis. But they provided useful information in only half of the patients with OAB. Therefore, today a comprehensive urodynamic study (KUDI) is prescribed in the following cases:
- difficulty in making a diagnosis;
- mixed type of urinary incontinence;
- previous operations on the pelvic organs;
- concomitant diseases of the nervous system;
- treatment failure;
- planning potentially difficult treatment, such as surgery;
- suspected neurogenic hyperactivity.
If neurogenic hyperactivity is suspected, the neurologist should also prescribe the following examinations:
- study of somatosensory evoked potentials;
- magnetic resonance or computed tomography of the brain and spine.
Treatment
OAB therapy is not well developed. This is due to the diverse clinical picture and the individuality of manifestations. In addition, the drugs used are often ineffective and toxic.
The main directions of treatment:
- non-drug;
- medicinal;
- surgical.
Behavioral therapy is used both on its own and in combination with medication. It lies in the patient's habit of controlling his bladder, treating him like a naughty child who must be carefully monitored. It is necessary to urinate at regular intervals during the day, increasing them more and more. Such training is especially useful for weakened urges and incontinence.
At a young age, Kegel exercises are recommended. Many women have known them since childbirth, when they used them to train their pelvic floor muscles. These techniques will also train the muscles around the urethra.
Behavioral therapy and physical therapy have practically no contraindications, they are harmless and free, which allows them to be recommended to the vast majority of patients.
Surgical treatment includes the following operations:
- denervation of the bladder (cessation of transmission of impulses that cause detrusor contraction);
- detrusor myectomy, which reduces the area of the overreactive muscle surface;
- intestinal plastic, in which part of the bladder wall is replaced by an intestinal wall that is not capable of imperative contractions.
Such operations are complex and are carried out only according to individual indications.
 Effective drug
Effective drug The basis for the treatment of patients with OAB is drugs. Of these, anticholinergics are the leading ones. Their action is based on the suppression of muscarinic receptors responsible for the contraction of the bladder muscle. Blockade of receptors causes a decrease in muscle activity, OAB symptoms decrease or disappear.
One of the very first drugs in this group is oxybutynin (Driptan), developed in the middle of the last century. It is quite effective, but has a number of adverse effects: dry mouth, blurred vision, constipation, palpitations, drowsiness and others. Such adverse events led to the search for new forms of drug administration: transrectal, intravesical, transdermal. A slow-release form has also been developed which, for the same efficacy, is markedly better tolerated and taken once a day. Unfortunately, it is not yet registered in Russia.
Trospium chloride is also widely used. In terms of effectiveness, it is close to oxybutynin, but is better tolerated. Its efficacy and safety are clinically proven.
Specially designed for the treatment of OAB tolterodine. In terms of effectiveness, it is comparable to the first two means, but is much better tolerated. The drug has been well studied. Its optimal dosage is 2 mg twice a day. There is also a slowly released form of the drug, which is much less likely to cause dry mouth. This form can be used in a large dosage, which allows you to completely get rid of the symptoms of the disease.
Tolterodine has the following contraindications:
- urinary retention (more common in men);
- untreated angle-closure glaucoma;
- myasthenia gravis;
- ulcerative colitis in the acute stage;
- megacolon (intestinal enlargement).
In all other patients, all symptoms are significantly reduced after 5 days of admission.
The maximum effect is shown in 5 8 weeks of reception. However, to maintain it, you must constantly take these drugs. Their cancellation will lead to a relapse of the disease.
Another possible effect after the use of any anticholinergic drugs, including tolterodine, is a violation of bladder contractility. There is an incomplete emptying of it, which can cause permanent urinary retention in the ureters and renal pelvis with subsequent development. Therefore, if there is a feeling of incomplete emptying of the bladder, patients receiving these drugs should immediately consult a doctor. When observing such patients, the volume of residual urine (not released during urination) should be measured using ultrasound monthly.
For symptoms of an overactive bladder in women, treatment is prescribed by a specialized specialist. This is a very urgent and delicate issue. This condition occurs quite often. This unpleasant symptom complex surpasses bronchial asthma, diabetes mellitus, and osteoporosis in frequency. About 17% of the adult population in the world has this disease. In both sexes, this disease occurs with the same frequency.
The mechanism of the disease
An overactive bladder is a characteristic syndrome. From 5 to 7 acts of urination per day is considered the norm. If the number of urination in the daytime is more than 8 times, this is a sign of overactive bladder syndrome.
If a person is forced to get up at night to urinate, this is also considered a pathological symptom.
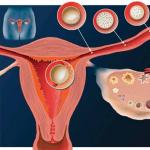
Inflammatory phenomena are absent. Violations occur in the lower urinary tract. In the filling phase of the bladder, its muscle (detrusor) suddenly begins to contract involuntarily. Pressure rises in the bladder. The woman suddenly feels the need to go to the toilet. The patient cannot stop the urge.

An overactive bladder in women is dangerous because it potentiates the ascending pathway of infection, affecting the kidneys. High pressure in the detrusor affects the upper urinary tract. This can lead to dysfunction, normal functioning of the kidneys. To fully live, the patient has to use various pads, diapers. For a woman, this is especially dangerous because the vagina is nearby. Incorrect padding damages the skin, the flora in the vagina is disturbed. Colpitis develops. To avoid complications, it is important to treat such an unpleasant pathology in a timely manner.
Etiological factors of pathology
 To date, the cause of this syndrome has not been identified. There are a lot of theories, but so far none of them is leading. Some scientists believe that past inflammatory diseases lead to such a pathology. Their opponents call hereditary factors as the cause of this syndrome. Scientists continue to work on this problem.
To date, the cause of this syndrome has not been identified. There are a lot of theories, but so far none of them is leading. Some scientists believe that past inflammatory diseases lead to such a pathology. Their opponents call hereditary factors as the cause of this syndrome. Scientists continue to work on this problem.
Provocative factors of pathology:
- neurological diseases. There is a violation of innervation. Neurogenic detrusor hyperactivity develops.
- Involvement of the nervous system leads to increased excitability and the occurrence of overactive bladder syndrome.
- Hormonal changes in the body. Very often, such symptoms occur in women in various periods of menopause. The older the woman who is in this condition, the more pronounced estrogen deficiency. Symptoms of urgency are more common in these women.
- anatomical changes. In some organic diseases, something interferes with the normal outflow of urine.
Clinical picture
The main symptom of this pathology is urgency. It is a sudden irresistible urge to urinate. The patient is unable to tolerate and control urination. The number of day and night acts of emptying the bladder increases. Characteristically accelerated.

In advanced cases, the symptoms are very severe. For such patients, even 20 ml in the bladder is a big problem. Pathology significantly affects the quality of life of a woman.
Diagnostic studies
Before starting treatment, it is important to conduct a correct differential diagnosis. It must be precisely established that this is not a stressful urgency.
If necessary, a young patient is sent for examination to a neurologist, since multiple sclerosis can debut with urination disorders.
 It is necessary to exclude the inflammatory process. It is important to distinguish this syndrome from cystitis. Patients with overactive bladder never experience pain. With cystitis, speeding up occurs. In patients with signs of urgency, urinalysis is normal. A tomographic study of the lumbosacral spine is being performed. To exclude tumor processes, an ultrasound examination is prescribed. It is very helpful to fill in a urination diary. This allows you to understand the essence of the existing problem.
It is necessary to exclude the inflammatory process. It is important to distinguish this syndrome from cystitis. Patients with overactive bladder never experience pain. With cystitis, speeding up occurs. In patients with signs of urgency, urinalysis is normal. A tomographic study of the lumbosacral spine is being performed. To exclude tumor processes, an ultrasound examination is prescribed. It is very helpful to fill in a urination diary. This allows you to understand the essence of the existing problem.
Treatment for an overactive bladder
Once the diagnosis is made, the specialist can start treating the patient.
Nowadays, drug therapy of this disease is being successfully carried out. In order to treat overactive bladder in women, effective methods have been developed.
Conservative treatment
The following activities are considered effective:
- M-anticholinergics are the main drugs. These antimuscarinic drugs block special receptors that carry out signal transmission. These receptors are located inside the bladder.
- The muscles of the urinary tract relax due to the use of beta3-adrenergic agonists. They quickly soothe the bladder, improve the elasticity of its walls. These drugs are very effective.

- The mucous membrane of the genitourinary system immediately reacts to a decrease in the level of sex hormones, therefore, specialists often prescribe hormonal preparations for women of the older age group. Local treatment with the use of medicines in the form of suppositories, creams helps a lot.
- Physical therapy helps a lot. Doctors prescribe electrical stimulation. In this case, a weak electric current irritates the nerve roots of the bladder. As a result, unstable contractions of its walls are suppressed.
- In the early stages of the disease, gymnastics can help, which strengthens the muscles of the pelvic floor. This is an effective bladder workout. It is useful to gradually increase the intervals between urination acts, imposing a certain rhythm of work on the organ.
- Proper nutrition is important. The patient needs foods that contain a lot of calcium. Hard cheese is the best source of this trace element. It promotes contraction of the pelvic floor muscles.

- Favorable conditions for the work of the bladder create bran, cranberries, sea buckthorn. Cheese contains a lot of magnesium, which is necessary for muscle relaxation. If there is enough trace element in the blood, then bladder hypertonicity does not develop. Spicy and salty foods, coffee, carbonated drinks irritate the body and interfere with its normal functioning.
- It is very important to choose the right pad or diaper. Hygiene products used by women during menstruation are not suitable, since a special diaper must be breathable.
 Botulinum toxin injections are one of the modern treatments for overactive bladder syndrome. The drug is injected directly into the wall of the bladder. For this, special endoscopes are used.
Botulinum toxin injections are one of the modern treatments for overactive bladder syndrome. The drug is injected directly into the wall of the bladder. For this, special endoscopes are used.
These devices for endoscopic surgery are introduced into the organ under vision control. Then, injections are performed with a special needle, which can be repeated after the end of the drug. Such manipulations allow you to block the transmission of an impulse from the nerve ending to the muscle. The supply of the substance that is responsible for these processes is stopped. In fact, part of the nerve endings is blocked. This condition is called chemical denervation in urology.
There is an effect of eliminating the hyperactivity of the bladder. At the same time, the effect of innervation is preserved, the bladder is viable.
After the use of botulinum toxin, control over urination is significantly improved.
Injections do not lead to organic changes in tissues, sclerosis of the organ. This fact has been proven through numerous studies.
If there is a positive trend, drug treatment should be continued. Such a course is assigned individually. If the disease is not amenable to drug therapy, the next step may be the use of sacral stimulation, the use of InterStim.

During surgery, an electrode is inserted into the sacral plexus, special sensors are connected. First, a testing phase is carried out, during which the doctor selects a dose of a nerve impulse for the patient.
Surgery
In advanced cases, when all conservative methods do not help, complex operations are performed. This treatment is rarely used. In the process of cystoplasty, the bladder is enlarged. The capacity of the organ increases due to part of the intestine.
During other complex surgical interventions, part of the muscles of the bladder is removed. However, such surgical treatment is indicated for a very small number of patients.
If female representatives have noticed symptoms of trouble in themselves, it is necessary to contact a therapist, urologist or gynecologist. This problem is solved in a complex way. Each clinical case is individual, so treatment can only be prescribed by a doctor. It is necessary to contact him in time.
A painful condition in which the patient urinates independently of his will is an overactive bladder in women, the treatment of an overactive bladder includes a number of methods, ranging from changing habits and behavior, pharmacotherapy, treatment with folk remedies and ending with surgery.
Syndrome Definition
Overactive Bladder Syndrome is a disease in which there are many symptoms, such as frequent urination and urination at night. The most important symptom is the excretion of a small amount of urine, regardless of the will of the patient.
The prevalence of overactive bladder in European society is estimated in the scientific literature at an average of 16%. According to various studies based mainly on survey results, the incidence remains between 7 and 30%.
This disease is slightly more common in women. The prevalence of overactive bladder increases with age, most commonly affecting people over 60 years of age. In epidemiological studies, the most common symptom in patients is pollakiuria - 85%, and urinary incontinence occurs in more than half of patients.
The cause of this violation has not been fully investigated. The group of symptoms of overactive bladder is caused by systolic instability of the detrusor, which leads to its increased sensitivity and more frequent contractions, the innervation of the bladder is disturbed.
An overactive bladder is diagnosed based on the patient's symptoms. Diagnosis of this disease is based mainly on the anamnesis and the establishment of a group of diseases reported by the patient. In addition, the diagnosis of an overactive bladder is possible only after the exclusion of other diseases of the genitourinary system, which can cause symptoms of pollakiuria and nocturia.
Treatment Methods
Treatment for an overactive bladder includes the following:
- conservative treatment;
- treatment with hormones (estrogens);
- the use of botulinum toxin;
- neuromodulation;
- pharmacotherapy.
In addition to excluding other diseases, an important element of diagnosis is familiarization with the patient's regimen. If the patient drinks a large amount of liquid before going to bed, then he will be forced to urinate at night, which will not be a symptom of the disease for him, but only a consequence of his behavior.
- Restriction of fluid intake, in addition to the situation of thirst, and caffeine intake is one of the elements of behavioral treatment. Another treatment is bladder training. It consists in increasing the intervals between emptying by periods of 30 minutes until reaching 3 hours. Such training lasts several weeks, but brings good results.
- In patients with urinary incontinence, an important element of conservative treatment, as well as an addition to other methods of treatment (pharmacotherapy, surgery) is the rehabilitation of the pelvic floor muscles. It consists in performing the so-called Kegel exercises. These are exercises to strengthen the pelvic floor muscles, proposed by Arnold Kegel, an American gynecologist, in the 50s of the XX century. They consist in tensing the pelvic floor muscles for a period of 8-10 seconds and repeating this procedure. The number of repetitions increases during subsequent exercises. There is no one scheme for the number of repetitions of these exercises. A professor of medicine who specializes in pelvic floor statics suggested a regimen of 3 to 12 repetitions over 3 months. Only 20% of women are able to properly stretch the muscles surrounding the vagina and rectum, the rest of the women, trying to perform Kegel exercises, strain the muscles of the abdomen and buttocks. Therefore, the woman must not only be instructed how to do the exercises, but also must be checked for the correctness of the exercises.
- If the patient is not able to perform Kegel exercises correctly, electrical stimulation can be used, which, however, is less effective than self-exercise exercises.
- In patients with atrophy of the genitourinary system, preparations containing estrogen for topical use, that is, vaginally, are used. This can effectively relieve the symptoms of an overactive bladder in post-menopausal women.
- In the absence of efficacy or the possibility of using pharmacotherapy and other methods of treatment, an injection using botulinum toxin into the wall of the bladder can be used. Botulinum toxin is a potent neurotoxin that inhibits the secretion of acetylcholine (a neurotransmitter) from nerve endings, resulting in detrusor diastole. This operation is performed in a hospital, under general anesthesia. The patient is placed in the same position as during a gynecological examination, then a cystoscope is inserted into the bladder, and botulinum toxin is injected into the wall of the bladder using a special needle. The effects of the treatment wear off within a few months. Urinary retention can be a complication after surgery.
- Neuromodulation is the inhibition of detrusor activation by electrical stimulation of nerve endings. The patient undergoes a procedure for implanting a special stimulator, similar to a pacemaker, in the vicinity of the ilium, and the electrode from the stimulator is inserted in the vicinity of the sacrum. The exact mechanism of action of this method has not yet been fully understood. This method is used for patients with persistent symptoms that do not respond to other methods of treatment.
Used medications
Medical therapy is the most commonly suggested treatment for overactive bladder. The main group of drugs are antimuscarinic drugs, i.e. blockers of muscarinic receptors from M2 and M3, which are located in the bladder. Blocking these receptors leads to relaxation of the detrusor, which leads to a decrease in painful symptoms and a decrease in the frequency of urination. Muscarinic receptors, in addition to the bladder, are located in various tissues of the body, and therefore their exclusion leads to rather burdensome side effects, such as: dry mouth, vaginal dryness, blurred vision, constipation, headaches, heart rhythm disturbances , severe symptoms of peptic ulcer, the occurrence of urine after urination. 
The severity of these symptoms, especially dry mucous membranes, is so severe that many people refuse treatment because of it. The following active substances of this group of drugs are distinguished: tolterodine, fesoterodine, solifenacin. The new generation drug in this group is solifenacin, which is characterized by a long battery life and is more selective in relation to receptors located in the bladder, and therefore causes fewer complications and is better tolerated by patients.
A new group of drugs used in the treatment of overactive bladder are beta-adrenergic agonists.
The b3 receptors are responsible for the relaxation of the detrusor during the filling phase of the bladder. Stimulation of these receptors leads to a decrease in detrusor tension, an increase in bladder capacity, and a decrease in the number of urination. The active substance in this group of medicines is mirabegron. Side effects that occur with the use of drugs from this group occur less frequently than in the case of the use of antimuscarinic drugs.
Before using a suitable method of therapy, the doctor must exclude the presence of other diseases that can give symptoms of an overactive bladder. Proper treatment relieves the patient from painful symptoms.
An overactive bladder is a pathology that is most often encountered by women and the elderly. This violation significantly worsens the quality of household, professional and social life. Many patients, embarrassed to go to the doctor with this delicate problem, try to pick up drugs for themselves at home, which only exacerbate the disease. In order to get rid of unpleasant symptoms, it is important to undergo a course of treatment, which can only be selected by a doctor, after a thorough diagnosis.
A person normally excretes about 2 liters of urine per day for 8 urinations. These figures may vary slightly, depending on the amount of liquid drunk and environmental conditions. The process of filling and emptying the bladder is controlled by the kidneys, pelvic muscles and the nervous system. Violation of the function of one of the systems that control urination leads to the phenomenon of hyperactivity.
In the ICD-10, this disease is under the code N32.8 - other specified lesions of the bladder.
The symptoms of this pathology are:
- increased urination more than 8 times a day, in the absence of excessive fluid intake;
- nocturia - the appearance or increase in imperative urges more than 2 times during the night, which causes insomnia and nervousness;
- the desire to urinate, even with an incomplete bladder;
- urge to urinate immediately after a previous visit to the toilet;
- a strong desire to urinate, appearing suddenly;
- that occurs after an imperative urge, in response to irritating factors - the murmur of water, loud sounds, fear.
Important! In hyperactivity syndrome, patients visit the toilet more often, while changing not the daily volume of urine, but its amount released at a time.
Diagnostics
The most common sign by which hyperactivity can be suspected is frequent urination, which sometimes leads to complete disability of the patient. It is with this problem that exhausted patients turn to therapists, gynecologists and urologists.

To make a diagnosis, doctors carefully collect an anamnesis, listen to all complaints and carefully examine the patient. In order to start treatment, it is necessary to accurately establish the cause leading to unpleasant manifestations.
For this purpose, use:
- Urination diary. The patient, for at least 3 days, must directly note the time of urination and urges for them, the amount of fluid excreted and drunk. It is also important to report episodes of incontinence and the number of pads used.
- Gynecological examination. In this case, a cough test or a straining test can be performed, in which the mobility of the pelvic organs is determined.
- Clinical blood test and urinalysis, which can be used to diagnose inflammatory processes in the body.
- Ultrasound examination of the kidneys and pelvic organs.
- Comprehensive urodynamic study, including cystometry, electromyography, urofluometry.
- Neurologist's consultation with suspicion of neurogenic hyperactivity.
- MRI or CT of the brain, spine and pelvis, in case of difficulty in making a diagnosis or suspicion of the presence of neoplasms.

Important! It is necessary to provide the attending physician with information about all the drugs taken. Many drugs used to treat hypertension or diabetes can cause more frequent urination.
How to treat hyperactivity
There is no generally accepted treatment regimen for hyperactivity. This is due to the variety and intensity of clinical manifestations, as well as the fact that various diseases lead to the emergence of this pathology. Depending on this, conservative and surgical treatment of OAB is distinguished. Also, behavioral therapy, which in mild cases can be used independently, and in severe cases, it complements the treatment prescribed by a specialist.

The gold standard is drug therapy. With its help, you can increase the functional capacity of the bladder, reduce the frequency and intensity of urges, and eliminate the episode of incontinence. Specialists prescribe the following drugs to patients with GABA:
- Trospium chloride, which belongs to the group of anticholinergic, antispasmodic drugs. In the body, it reduces the tone of smooth muscles, as well as the frequency of urinary contraction, thereby reducing the frequency of the urge to urinate. It also eliminates urinary incontinence.
- Tolteradine. A drug specifically designed for GABA therapy. It leads to an increase in the intervals between urination, weakens imperative urges, suppresses unintentional urination. Symptoms of the disease when taking this drug are reduced by day 5, and the therapeutic effect occurs after 3-4 weeks of administration.
- Resiniferoxytin- used in neurogenic hyperactivity. It is introduced into the cavity of the bladder, where it suppresses the sensitivity of receptors that send signals to the brain about the need to empty.
- Botulinum toxin- is widely used by many specialists. It is introduced into the smooth muscles of the bladder, causing its temporary paralysis and a decrease in contractile activity. The effect of the drug lasts from 3 to 10 months.
- Anti-inflammatory drugs, antibiotics prescribed for OAB caused by infectious processes in the pelvic organs.
Usually drug therapy lasts 3 months, after which the effect lasts for several months. It is important not to stop the use of non-drug methods or start them in order to consolidate the achieved effect.
Surgical intervention for OAB
With the ineffectiveness of conservative treatment, frequent relapses or severe urinary incontinence, doctors may recommend surgery for the patient.
To eliminate the symptoms of OAB, surgical techniques are used such as:
- bladder denervation;
- detrusor myectomy;
- intestinal plastic, in which part of the bladder wall is replaced by intestinal tissue that does not carry sensitive receptors.
Important! Indications for surgical intervention are determined strictly on an individual basis. With the ineffectiveness of conservative therapy, with the unwillingness or impossibility of performing an operation, the method of neuromodulation can be used. It is based on the impact on the vesical muscles by weak electrical impulses, leading to a decrease in its contractile activity.
Non-pharmacological help
Behavioral therapy is one of the most important components in the treatment of OAB in women. It can be used both independently, with minor manifestations of pathology, and in combination with drugs.
To reduce unpleasant manifestations, you should:
- Follow a special diet. It is necessary to exclude from the diet foods that lead to irritation of the bladder mucosa - coffee, spicy and sour foods, carbonated mineral water, alcoholic beverages.
- Limit, and do not use watermelons, cucumbers, melons for the duration of treatment.
- Observe the drinking regimen, drink enough fluids. Do not drink at night.
- Engage in special physical therapy. For this purpose, Kegel exercises, familiar to many women as gymnastics to strengthen the pelvic muscles, are suitable.
- Follow a specific regimen of emptying, agreed with the attending physician. You need to urinate at certain intervals, thereby correcting the prevailing pathological stereotype.
Important! With OAB, you can not self-medicate. Proper nutrition, physiotherapy exercises and therapy, effectively selected by a specialist, can quickly eliminate discomfort. Compliance with these conditions leads to a successful recovery and prevents the occurrence of chronic forms of the disease.
Information about an overactive bladder, the occurrence of the disease, diagnosis and treatment in this video.
No specialist can give an unequivocal answer to the question of what exactly provoked the development of the disease in a particular person, whether it be a woman or a man. After all, even a thorough examination does not allow you to get a complete picture.
However, there are a number of factors, the presence of which most often provokes the development of such a violation:
- consumption of large amounts of fluid in the presence of abnormalities in the work of the kidneys;
- development of acute infectious processes of the urination system;
- the course of an inflammatory, infectious process near the bladder;
- diabetes;
- the presence of other reasons due to which the outflow of urine is disturbed - constipation, stones in the urinary tract, the presence of a tumor, the consequences of surgical interventions on the pelvic organs;
- malfunctions of the nervous system (sclerosis, Parkinson's disease);
- cardiovascular diseases, strokes;
- hormonal changes during menopause;
- senile age, when the brain does not recognize the signals coming from the body;
- the presence of benign neoplasms of the prostate gland (in men);
- abuse of alcohol, drugs, smoking;
- incomplete emptying of the organ during urination, which entails a decrease in free space for new portions of the urinary fluid;
- constant or episodic use of medications - diuretics.
Often, an overactive bladder is diagnosed as a congenital pathology of the structure of the urinary canal. And stressful situations and work in harmful conditions only exacerbate the situation and further intensify the process of disease development.
During the period when a woman is carrying a child, an overactive bladder is a consequence of the effect of the fetus on the organ of the excretory system.
Most experts suggest that a decrease in the number of M-cholinergic receptors (denervation) leads to the development of pathology. This causes a decrease in the influence of the nervous system on the smooth muscle cells of the bladder, as a result of which close contacts are formed between them.
As a result, the impact of a nerve impulse on a small section of the muscle wall is accompanied by a rapid spread of excitation to all myocytes, their sharp contraction, which causes an imperative (urgent, uncontrolled) urge to urinate.
Clinical picture of the disease
The disease of overactive bladder can be diagnosed independently, if you know the main symptoms of the manifestation of the disease:
- frequent urination during the day (more than 8 times, of which 2 or more occur at night);
- involuntary release of urine (incontinence);
- sudden and rather strong urge to urinate (often ending in the release of a small amount of urine).
The above signs indicate a serious health problem and the need to take measures to stabilize the genitourinary system.
Indeed, in addition to the fact that this circumstance leads to a limited movement of a person, it also affects the psycho-emotional state and a decrease in self-esteem, which is often accompanied by a depressive state.
Specialists distinguish several forms when the organ of the urination system is hyperactive - idiopathic and neurogenic.
In the first case, it is almost impossible to determine the factor that provoked the exacerbation of the organ of the genitourinary system.
The second form is a consequence of disorders of the nervous system.
At the same time, it is impossible to exclude the possibility that infectious and other diseases act as a provocateur of urinary incontinence and the transformation of an organ of the urination system into a hyperactive mode.
Features of an overactive bladder in children
In young children, neurogenic overactivity of the bladder is manifested by the following symptoms:
- frequent urination (more than 8 times a day) in small portions;
- imperative urges;
- urinary incontinence (enuresis).
The postural form of overactive bladder in children is manifested by daytime pollakiuria with normal nocturnal accumulation of urine.
Girls may experience small amounts of urine during puberty during exercise (stress urinary incontinence).
Symptoms of neurogenic urinary disorders
A hyperreflex bladder is characterized by excessive detrusor tension. This condition has the following symptoms:
- increased urination, if normally it occurs up to 8 - 10 times a day. Their number may fluctuate depending on the amount of fluid drunk, alcohol consumption or diuretic intake. But a persistent increase in the number of urges to urinate more than 8 - 9 times during the day and 3 - at night indicates a violation of the detrusor;
- the urge to urinate is formed even with insufficient filling of the bladder, that is, the total daily volume of urine excreted remains the same;
- the inability to restrain the desire to urinate, up to partial or complete urinary incontinence;
- "Double" urination, that is, after the process of urination is over, you can continue it by straining.
Women and men experiencing overactive bladder syndrome may have one, two, or all of these symptoms.
The main manifestations of the syndrome are:
- increased daytime and nighttime urination;
- urinary incontinence;
- pain in the lower abdomen;
- a feeling of fullness of the bladder, which persists even after going to the toilet.
Diagnostics
The above symptoms may also appear with some inflammatory lesions of the bladder, such as cystitis, and "double" urination may indicate the presence of a diverticulum.
In addition, the cause of a hyperactive disruption of the detrusor is very important. Therefore, all further treatment depends on the results of diagnostic procedures.
To exclude bacterial inflammation, clinical blood and urine tests are done. The assessment of the anatomical structure of the lower urinary system and the condition of the prostate gland in men is done according to the results of ultrasound, CT or MRI.
The assessment of urodynamics plays a decisive role in the diagnosis of an overactive bladder. For this, the following methods are used.
When conducting urofluometry, the volume of urine excreted, the flow rate and the duration of the urinary process are assessed.
More indicative is the method of cystometry, which allows you to determine the values of intravesical pressure and total pressure in the abdominal cavity when filling the bladder. To do this, the organ is filled with a special solution through the catheter.
In this case, the patient should be in a standing position. When the urge to urinate cannot be contained, the necessary measurements are taken. During urination, its volumetric velocity is also measured.
The contractile functions of the sphincters of the urethra are determined using profilometry. Especially this study helps to diagnose the cause of an overactive bladder in men with prostatic hyperplasia.
There is not enough data provided by the patient to make a correct diagnosis. Some of these symptoms of an overactive bladder are similar to those of other urinary tract diseases.
It is rather problematic to differentiate the disease without a detailed study, since cystitis has similar symptoms, and, for example, “double” urine output often indicates the presence of a diverticulum.
In addition, the main cause of the development of hyperactive syndrome is of great importance.
In addition to the "standard" urinalysis, patients with complaints of frequent urination, with suspicion of increased bladder reflexivity, are prescribed ultrasound, and, if necessary, MRI, CT. The following laboratory methods are used for determination:
- urofluometry - gives an objective assessment of the volume, speed and duration of its excretion from the body;
- cystometry - determines the level of pressure inside the organ, as well as the abdominal cavity when the latter is filled;
- profilometry - allows you to verify the functionality of the urethral sphincters, more often used in men.
Diagnosis of an overactive bladder is based on the identification of characteristic signs of pathology, instrumental and laboratory examination data.
When examining children with an overactive bladder, it is necessary to clarify the characteristics of the course of childbirth, the presence of a hereditary predisposition.
In order to exclude diseases of the genitourinary system of an inflammatory nature, patients are prescribed:
- general blood analysis;
- general urine analysis;
- biochemical analysis of blood and urine;
- Zimnitsky's test;
- urinalysis according to Nechiporenko.
Instrumental diagnosis of an overactive bladder:
- cystoscopy;
- ultrasound examination of the kidneys and bladder;
- radioisotope renography;
- ascending pyelography;
- excretory urogrophy;
- voiding and conventional urethrocystography;
- uroflowmetry;
- profilometry;
- sphincterometry;
- cystometry.
Treatment
It is worth noting that such a syndrome is not only a medical, but also a big psychological problem. An overactive bladder can drastically affect a person's lifestyle, especially if it is accompanied by urinary incontinence.
Therefore, the full treatment of hyperactive syndrome should also include the competent work of a psychologist and the help of relatives.
The main treatment for overactive bladder in men and women should be directed at combating the underlying cause of the condition. However, in some cases, the treatment of the "main" disease for a number of reasons is impossible.
In any case, doctors prescribe symptomatic treatment. To do this, drugs are used that can "slow down" the formation of urine, thereby physiologically reducing the need for frequent visits to the toilet.
The contraction and relaxation of the detrusor occurs when exposed to specific receptors in the wall of the bladder.
The appointment of drugs that, depending on the indications, block or, conversely, stimulate these nerve endings, help to normalize the work of the muscles of the bladder.
In severe cases, an overactive bladder is treated with surgery. Basically, during the operation, flaps of high-tech synthetic material are sewn in, which support the muscles of the organ.
In addition to drug therapy, physiotherapy is also very effective. Usually used various methods of electrical stimulation and acupuncture.
An overactive bladder is almost always accompanied by stagnation of urine, which is the cause of the development of bacterial inflammation.
Therefore, in order not to have to treat cystitis later, it is better to carry out preventive treatment with uroseptic drugs or antibiotics.
If it is impossible to cure the disease conservatively, resort to the help of a surgeon. Surgery is often indicated on a case-by-case basis and is not a mandatory treatment for overactive bladder.
Among the manipulations that are used in this disease, it is worth noting several surgical procedures.
The first is the denervation of the organ, aimed at stopping the transmission of neural impulses, because it is they that affect the contraction of the walls.
The second variant of surgical treatment is myectomy, which implies a reduction in the area of the receptive surface of the detrusor by its partial removal.
Intestinal plastic is the replacement of the walls of the bladder with intestinal walls that are not capable of contraction.
Physiotherapists are confident in the need for physiotherapy with an overactive bladder. Over the past decades, acupuncture and electrical stimulation procedures have proven themselves to be excellent.
The bladder, which is hyperactive in both men and women, requires complex treatment, including both the use of medicines and folk remedies.
To date, there are a fairly large number of medications, the use of which has a positive effect on the state of the genitourinary system.
Depending on the severity of this pathology in a particular patient, as well as the characteristics of the body, the attending physician selects drug therapy, which involves the use of such groups of drugs:
- m-anticholinergics, adrenoblockers (Oxybutynin, Tolterodine, Trospium, Solifenacin);
- antidepressants (amitriptyline, imipramine);
- toxins (botulinum toxin).
For older patients, hormonal preparations are selected, the main purpose of which is to compensate for the estrogen deficiency. At the same time, other concomitant diseases are taken into account.
Any medication has both indications for use and contraindications. This fact must be taken into account in the process of prescribing a particular drug.
Moreover, if after the start of taking there are no obvious improvements, but there is a general malaise and malfunctions of other organs, then you should immediately contact your doctor to change therapeutic prescriptions to more acceptable ones.
Surgery
After the examination, the clinical picture of the disease will become more clear and detailed for the attending physician, which will allow him to draw up an appropriate therapeutic regimen.
Since the treatment of an overactive bladder requires a comprehensive, thorough approach, the patient should seriously approach each prescribed event, taking the drug.
In addition, most experts consider this syndrome not only a physiological, but also a psychological disorder.
If we take into account the fact that the work of a hyperactive organ significantly affects the patient's well-being and lifestyle, then the treatment of the syndrome is the professional assistance of a urologist, psychologist, as well as the assistance of relatives and friends.
The first thing that forces should be thrown at is the elimination of urinary incontinence. To get rid of such an unpleasant symptom, it is important to deal with the root cause of its appearance.
But it is worth considering that it is far from always possible to treat the “main” pathology, especially if it belongs to the category of neurological or oncological.
In this case, the doctor prescribes palliative treatment aimed at improving the quality of life and eliminating the uncomfortable manifestations of hyperactive syndrome.
First of all, medications are prescribed that can reduce the functional formation of urine. Passing the course will reduce the frequency of urges and visits to the toilet.
Drugs such as Driptan, Tolterodine, Trospium chloride act directly on the receptors present in the detrusor of the patient's overactive urinary "reservoir" and help to normalize the functioning of the bladder muscles.
In parallel with these drugs, the patient is shown antibiotics and uroseptics. The syndrome of increased reflexivity in the predominant number of cases is accompanied by congestion in the bladder, which often serves as the basis for the development of a bacterial infection.
Active pathological activity of the bladder is treated in various ways. The main requirement is to learn to restrain the strong urge to urinate and try to control them.
The treatment will be carried out for a long period of time, which requires the patient to be patient and unquestioningly follow the doctor's recommendations.
As a therapy, the doctor may prescribe the following measures:
- the strictest diet, which provides for the intake of healthy food in optimal quantities (fried, fatty, overly salty, spicy foods are excluded);
- the right way of life and the rejection of bad habits;
- regulation of the state of the nervous system by taking antidepressant drugs;
- drawing up the correct daily routine - alternating the period of work and rest;
- weight control, since people with obesity often have a problem with frequent urination;
- restriction of fluid intake, often drawing up a special schedule, according to which it will be possible to drink drinks at an agreed time in a specified amount;
- performing a set of physical exercises to strengthen the muscles of the pelvic floor. Strengthening the muscles and maintaining it in good shape will allow for many years to get rid of involuntary and frequent contractions of the bladder.
Despite the effectiveness of the above methods, after undergoing therapy, not everyone manages to forget what an overactive bladder is in women, the treatment of which was carried out according to the most loyal scheme.
Each case is considered individually and requires a special approach to healing.
- with a certain frequency, perform the procedure for forced descent of urine using a catheter. However, one should be extremely careful, this method of emptying should be carried out only in medical institutions under the guidance of qualified specialists;
- wear special urological pads or absorbent underwear. In unforeseen situations, such precautions will protect outerwear from "leaks";
- exercise your bladder. This method involves going to the toilet on a schedule. You need to start with 30 minutes and gradually increase the interval. Of course, the patient will need to show patience and willpower, since such trainings must be carried out for a long period.
There are not isolated cases when none of the available methods does not provide the desired result. An overactive bladder in some women requires surgical treatment.
Correction of one's own behavior is one of the main methods of dealing with overactive bladder. People with this disorder develop a special pattern of behavior.
They literally become dependent on the toilet, cannot plan long trips, walks, and always run to the restroom before leaving the house. The elimination of such behavioral features should be performed by the patient independently.
This will help regain lost control over urination and manage how often you go to the toilet.
.
Patients with OAB are encouraged to schedule toilet visits. In this case, it is necessary to gradually increase the time intervals between urination. This approach is an excellent training for the bladder and will help a person control one of the main physiological processes in his body.
Prevention measures
Prevention is always more appropriate than treatment of the disease, especially if there are frequent manifestations of pathological abnormalities.
Treatment of an overactive bladder in women can be completely avoided if you follow simple recommendations:
- annually undergo a preventive examination by a urologist for men and a gynecologist for women;
- at the first manifestations of the disease, immediately seek medical advice;
- do not exceed the allowable dose of fluid consumed;
- prevent nervous disorders;
- during pregnancy, make regular visits to an obstetrician-gynecologist;
- if we are talking about a child, then you should seek advice from a child psychologist;
- give up all bad habits.
You should be extremely attentive to your health and respond to distress signals in a timely manner. If you start treatment in the early stages of the development of the disease, you can avoid the transformation of a pathological deviation into a chronic form.
In addition, this will save not only precious time, but also financial resources, which often has a key impact on the course of treatment.
Diet and drinking regimen
It is worth noting that before treating an overactive bladder with medication, the doctor will determine the drinking regimen, as well as the diet and daily routine.
In particular, the therapy of the disease implies strict adherence to the fluid intake schedule.
The patient should not drink later than 2-3 hours before going to bed. The choice of drinks should be careful, because with hyperactive syndrome it is extremely important to prevent irritation of the walls.
Citrus fruits, coffee, tea, alcohol, energy drinks and carbonated drinks give the opposite effect - they must be flatly abandoned, replaced with cranberry juice, water with a neutral content of trace elements, herbal teas.
As for dietary restrictions, they concern salty and peppery foods, fatty and smoked foods, sweets and pastries. For the period of exacerbation, it is better to completely exclude pork, beef, as well as legumes and nuts from the diet.